Jhonny A. Salomon, M.D.
Albert S. Woo, M.D., M.B.
M. B. Freeman, M.D., Ph.D.
Author’s affiliation:
Brown Medical School
Rhode Island Hospital Department of Plastic Surgery
Providence, Rhode Island
BACKGROUND
Forehead rejuvenation procedures can lead to excessive elevation of the medial brow, resulting in the”surprised look.” Differential treatment of the medial and lateral brow allows more precise positioning. The purpose of this study was to determine whether retaining structures exist in the forehead that would permit this differential elevation.
METHODS
Anatomical dissections were performed in the foreheads of 12 cadavers. Multiplanar dissections at the subperiosteal, subgaleal, and subcutaneous levels were performed on eight hemiforeheads. Clinical correlation for these findings was obtained during endoscopic and open brow-lift surgery.
RESULTS
Four retaining structures of the brow were identified: three medial and one lateral. The superomedial attachment begins 13 mm from the midline and 10.8 mm above the supraorbital rim. The superolateral attachment begins 23 mm from the midline and 10.3 mm above the supraorbital rim. The inferomedial attachment begins 12.6 mm from the midline at the level of the supraorbital rim, just medial to the supraorbital nerve. These three structures were found to control the position of the medial brow. Laterally, brow position was controlled by a broad ligamentous attachment extending across the lateral aspect of the supraorbital rim.
CONCLUSIONS
Medial retaining structures have been found to extend from the cranium into the forehead musculature. Release of the lateral broad ligamentous attachment was performed, followed by selective preservation of medial retaining structures. With this approach, we were able to gain control of the position of the medial brow and prevent overelevation and lateral spreading. (Plast. Reconstr. Surg. 117: 95, 2006.)
The description of the facial retaining ligaments was instrumental in the development of corrective surgery for the aging face.1,2 Recent contributions to the literature by Mendelson and colleagues have systematically examined the anatomical structures of the midcheek, malar mounds, lower lids, temple, and periorbital regions.3-5 Byrd suggested the presence of similar structures in the forehead based on his clinical experience and anatomical findings in trauma patients who had sustained severe soft-tissue injuries of the forehead.6 Ligamentous structures associated with the forehead have previously been described.2,7,8 However, no such structures of the brow have been clearly documented in the literature. A precise anatomical description of brow and forehead retaining structures would allow greater versatility and control during forehead rejuvenation procedures.
Originally in forehead rejuvenation, the eyebrow was considered a single aesthetic unit. In general, however, a higher position of the lateral brow as compared with the medial brow is desirable in women. Although adequate repositioning of the lateral brow has been achieved, postoperative results from both endoscopic and open approaches have suffered from excessive medial brow elevation or lateral spreading. Such results have been characterized as the “surprised look.”9 This has been attributable to the wide amount of undermining in the medial brow region followed by a superolateral traction vector. A major challenge has been to keep the medial brow down while attaining exposure adequate to address the medial corrugator, the procerus muscles, and the glabellar rhytides. Differential treatment of the medial and lateral brows would allow for a more precise positioning of the forehead elements and yield a greater aesthetic balance in the result. The purpose of this study was to provide an anatomical description of the brow retaining structures and to examine whether their selective release during foreheadplasty would allow simultaneous control of the medial brow and adequate exposure in the glabellar region for an overall improved aesthetic result.
MATERIALS AND METHODS
Anatomical dissections were performed in the foreheads of 12 cadavers, some of which were fresh tissue specimens. Modified coronal and hairline incisions were used for exposure, and the foreheads were divided into two halves through the midline. Dissection of six cadavers (eight facial halves) was performed at multiple planes: subcutaneous, subgaleal, and subperiosteal.
The subcutaneous plane of dissection was first explored through the incision. The frontalis muscle was released from the overlying dermis and the dissection was continued caudally deep to the brow onto the upper eyelid orbicularis oculi muscle. The subgaleal plane was then addressed using careful spreading scissors dissection. The galea was elevated off the underlying periosteum and separated from the frontalis above. Lastly, the subperiosteal plane was dissected using a periosteal elevator down to a level just inferior to the supraorbital rim. The retaining structures at each level were recorded. Their relationships to each other, to the midline, and to the supraorbital rim were also measured. In two cadavers, dissection of both hemiforeheads was performed for side-toside comparison of the location of the retaining structures.
Clinical correlation for the findings from cadaver studies was established. Through numerous endoscopic and open brow-lift dissections, the position of the brow retaining structures was observed. Using both endoscopic and open techniques, the glabellar region was addressed and the medial retaining structures were left intact. The lateral retinacular attachments10 were divided lateral to the supraorbital nerve but not in the area of the medial retaining ligamentous structures.
RESULTS
Cadaver Dissections
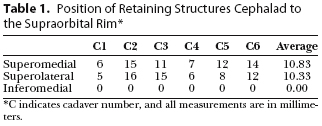
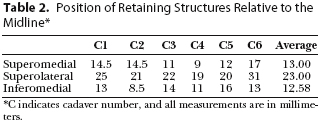
The dissection in the subperiosteal plane was performed with the periosteal elevator. Blunt dissection was accomplished easily until resistance was noted approximately 1 cm above the orbital rim. At this level, two attachments were identified: (1) a superomedial ligamentous attachment that originates on average 10.8 mm above the supraorbital rim and 13 mm from the midline and (2) a superolateral ligamentous attachment that originates on average 10.3 mm above the supraorbital rim and 23 mm from the midline (Fig. 1). Below the level of these two areas is a region where the periosteum is more easily elevated from the cranium. At the orbital rim, a third retaining structure exists: the inferomedial ligamentous attachment, which originates 12.6 mm from the midline. These areas do not have the same appearance as the more defined ligaments of the midface4,5 but rather are comparatively broadbased.
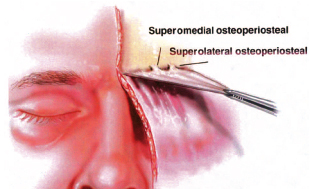
Fig. 1. Superomedial and superolateral ligamentous attachments are defined in the subperiosteal space. The superomedial structure averages 10.8 mm above the supraorbital rim and 13 mm from the midline. The superolateral structure averages 10.3 mm above the supraorbital rim and 23 mm from the midline.
At the subgaleal level, the dissection in the loose areolar plane was also undertaken. Two retaining structures were identified approximately 1 cm above the supraorbital rim. These two structures in the subgaleal space are a continuation of the previously described superomedial and superolateral osteoperiosteal attachments that are present in the subperiosteal space. Below these two structures is the subgaleal glide plane that extends for 1 cm until the margin of the supraorbital rim. At the orbital rim, just medial to the supraorbital nerve, there is another subgaleal structure that is a continuation of the previously described inferomedial attachment.
Dissection also identified the presence of a broad ligamentous structure extending across the lateral aspect of the supraorbital rim at the subgaleal level. This attachment continues onto the upper portion of the lateral orbital rim, where it is adherent to the superficial temporal fascia, as described by Knize.7,8 This entire structure, including its extension onto the lateral orbital rim, must be released to obtain optimal elevation of the lateral brow.
At the subcutaneous level, there were tight attachments of the skin to the frontalis muscle, presumably by the retinacula cutis. The dissection was performed sharply for the most part, and no definite retaining structures were identified in this plane. There was no glide between these two planes; the frontalis muscle and overlying skin always moved as one unit.
Comparison of both sides of each forehead was performed in two cadavers. The position of all three medial retaining structures was consistent between the two sides. Close anatomical correlation was demonstrable between sides of each individual cadaver. However, a wider range of values among differing individuals was noted (Tables 1 and 2).
Clinical Correlation
These findings were confirmed in further anatomical dissections. Additional fresh cadavers were used to evaluate the viability of surgical techniques for selective preservation of the medial retaining ligamentous attachments with release of the lateral brow elements. Hemiforeheads were dissected solely within the supraperiosteal plane. Lateral dissection and release of the broad lateral ligamentous attachment was initially performed. After this, the three medial structures were divided with complete release down to the supraorbital nerve. Mobility of the medial brow was dramatically altered with the additional dissection. [Note: Video of the mobility of the brow following each portion of the dissection may be observed by viewing this Journal online (Videos 1 and 2)].
In our clinical cases, we use the results of our laboratory study of the ligamentous attachment positions to preserve them with both open and endoscopic approaches. After the initial incision, dissection was performed in the supraperiosteal plan toward the supraorbital region. Care was taken to avoid dissection into the medial brow retaining structures. Dissection was made from lateral to medial across the superolateral orbit. The lateral retinacular ligament was released lateral to the supraorbital nerve. Adequate exposure to treat the medial corrugator and procerus muscles was achieved by dissecting a central tunnel between the two superomedial retaining structures (Fig. 6). Leaving these medial retaining structures intact allowed control of the position of the lateral brow and prevented overelevation and lateral spreading of the medial brow in both endoscopic and open procedures (below).


Preoperative and postoperative photographs of a patient who underwent endoscopic forehead rejuvenation, rhytidectomy, and upper and lower blepharoplasty. Corrugator transection and glabella rhytides were addressed while leaving the medial retaining ligaments down to prevent over elevation and lateral spreading of the medial brow. Special emphasis was placed on reshaping the right lateral brow.Note the evidence of left lateral eyebrow spreading that exists preoperatively.
Video 1: (Videos are available online at www.plasreconsurg.com.) Video revealing mobility of the brow following selective release of the broad ligamentous attachment along the lateral brow. Medial retaining structures have been left in place. Video 2. Similar video following complete release of the retaining ligamentous attachments. Note the increased mobility of the medial brow resulting in the surprised look.
DISCUSSION
Ligament versus Ligamentous Attachment
Some controversy has arisen regarding the appropriate terminology to be used for the differing retaining structures of the face. Although ligaments have traditionally referred only to connective tissue between bones, Furnas2 introduced the concept of “cutaneous retaining ligaments” as those elements in the craniofacial region that run from deep, fixed structures to the overlying dermis. This has gained wide support in the literature.11,12 As such, Knize has described the orbital ligament that tethers the lateral orbital rim to the superficial temporal fascia and dermis.13 This same ligament was later confirmed by Moss et al., and was referred to as the temporal ligamentous adhesion.3
Stuzin et al.11 expanded the definition of retaining ligaments further by classifying such structures into two groups: the true osteocutaneous ligaments and a second group of structures that serve as a coalescence between the deep and superficial fasciae of the face. The overlying skin is indirectly adhered to the structures by means of a closely adherent retinacula cutis. By using this expanded definition, Muzaffar et al.4 eloquently described the existence of the orbicular retaining ligament.
Knize13 advocated a more conservative approach to the naming of structures, suggesting that the term ligament should strictly refer to those structures that insert directly into the dermis. Although there is value to the preservation of strict anatomical criteria for the naming of newly discovered structures, it is difficult to deny the inherent value of recognizing those anatomical elements that influence the overlying skin indirectly through the retinacula cutis.
This study demonstrates the existence of structural attachments that assist in defining individual eyebrow shape and position. These structures are noted to arise from the cranium and insert at the level of the musculature, rather than the dermis. Dermal attachments are established through a closely adherent retinacula cutis. As this description does not fit the classic definition of a ligament, we have thus labeled them as ligamentous attachments.
Surgical Applications
Numerous studies concerning eyebrow aesthetics have shown that a lower position of the medial brow is desirable.14-16 Traditional techniques in brow-lifting surgery may cause unwanted medial brow elevation. It is our opinion that the most important factor leading to patients with the surprised look is wide undermining in the region of the central brow, with subsequent traction after release.
The corrugator, depressor supercilii, and orbital portion of the orbicularis oculi muscle are each depressors of the medial brow.17-19 They are all (to a certain extent) affected during brow-lift surgery. This is especially true of the corrugator muscle, which may frequently undergo myotomy or myectomy. Dysfunction of these medial brow depressors plays a role in central brow elevation. However, it is our experience that even without dissection of the central brow depressors, medial brow elevation can occur after brow-lift surgery if wide undermining has been performed. By leaving the medial brow retaining structures intact, we were able to control the position of the central brow even after extensive muscle alteration. These observations point to the key role that the medial brow retaining structures play in the control of the central brow.
The medial brow retaining structures also counteract the effect of gravity on the central brow. Ptosis of the brow commonly affects the lateral third of the brow to a greater extent and more prematurely than it does the medial brow.10,20 The pathogenesis of the slow aging process has been partially delineated by anatomical observations in the periorbital regions.3
Based on our observations, the three medial retaining structures provide excellent anchorage of the central brow to the frontal bone, thereby delaying the effect of gravity on the medial brow. Although there exists 1 to 2 cm of skin movement of the medial brow with active or passive motion, this movement occurs over the subgaleal glide plane in the area between the supero- and inferomedial ligaments. Thus, above the superomedial and lateral retaining structures and below the inferomedial structure, there is restricted motion of the medial brow skin. The superior and inferior structures permit motion in the 1-cm area over the medial eyebrow that they border but limit movement away from the anchor points. It is in this fashion that the effect of gravity on the central brow is limited.
Conversely, the lateral brow region is fixated primarily by the broad lateral ligamentous attachment, which extends across the lateral aspect of the supraorbital rim. This provides less anchorage than the three medial retaining structures. Thus, ptosis may develop earlier in lateral portions of the brow. Selective release of this structure, however, allows for significant lateral brow elevation without influencing the medial brow.
CONCLUSIONS
This study reveals that there consistently exist retaining ligamentous attachments of the medial brow and confirms the presence of the lateral ligamentous attachments. Those that are medial in location are paramount in the control of central brow positioning during forehead rejuvenation. We were able to incorporate this knowledge into our surgical treatment and thereby differentially shape segments of each brow.
Patrick K. Sullivan, M.D.
Division of Plastic Surgery
Brown Medical School
235 Plain Street, Suite 502
Providence, R.I. 02905
ACKNOWLEDGMENTS
The authors thank Rod Rohrich, M.D., and William Adams, M.D., for generous collaboration with this study, part of which was performed using fresh cadaver dissections from the laboratory at The University of Texas Southwestern Medical Center, Dallas, Texas. They also thank Ted Goslow, M.D.
REFERENCES
1. Furnas, D. W. Strategies for nasolabial levitation. Clin. Plast. Surg. 22: 265, 1995.
2. Furnas, D. W. The retaining ligaments of the cheek. Plast. Reconstr. Surg. 83: 11, 1989.
3. Moss, C. J., Mendelson, B. C., and Taylor, G. I. Surgical anatomy of the ligamentous attachments in the temple and periorbital regions. Plast. Reconstr. Surg. 105: 1475, 2000.
4. Muzaffar, A. R., Mendelson, B. C., and Adams, W. P. Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus. Plast. Reconstr. Surg. 110: 873, 2002.
5. Mendelson, B. C., Muzaffar, A. R., and Adams, W. P. Surgical anatomy of the midcheek and malar mounds. Plast. Reconstr. Surg. 110: 885, 2002.
6. Byrd, H. S. Personal communication, 1996.
7. Knize, D. M. An anatomically based study of the mechanism of eyebrow ptosis. Plast. Reconstr. Surg. 97: 1321, 1996.
8. Knize, D. M. The Forehead and Temporal Fossa: Anatomy & Technique. Philadelphia: Williams & Wilkins, 2001.
9. Rohrich, R. J. Limited incision foreheadplasty (Discussion). Plast. Reconstr. Surg. 103: 285, 1999.
10. Ramirez, O. M. Endoscopically assisted biplanar forehead lift. Plast. Reconstr. Surg. 96: 323, 1995.
11. Stuzin, J. M., Baker, T. J., and Gordon, H. L. The relationship of the superficial and deep facial fascias: Relevance to rhytidectomy and aging. Plast. Reconstr. Surg. 89: 441, 1992.
12. Zide, B. M. Surgical anatomy of the ligamentous attachments in the temple and periorbital regions (Discussion). Plast. Reconstr. Surg. 105: 1495, 2000.
13. Knize, D. M. Reassessment of the coronal incision and subgaleal dissection for foreheadplasty. Plast. Reconstr. Surg. 103: 1326, 1999.
14. Freund, R. M., and Nolan, W. B., III. Correlation between browlift outcomes and aesthetic ideals for eyebrow height and shape in females. Plast. Reconstr. Surg. 97: 1343, 1996.
15. Flowers, R. S., Caputy, G. G., and Flowers, S. S. The biomechanics of brow and frontalis function and its effect on blepharoplasty. Clin. Plast. Surg. 20: 255, 1993.
16. Bruck, J. C., Baker, T. J., and Gordon, H. Facial mimics and the coronal brow lift. Aesthetic Plast. Surg. 11: 199, 1987.
17. Isse, N. G. Endoscopic forehead lift. Clin. Plast. Surg. 22: 261, 1995.
18. Matarasso, A. Endoscopically assisted forehead-brow rhytidoplasty: Theory and practice. Aesthetic Plast. Surg. 19: 141, 1995.
19. Knize, D. M. Muscles that act on glabellar skin: A closer look. Plast. Reconstr. Surg. 105: 350, 2000.
20. Byrd, H. S., and Andochick, S. E. The deep temporal lift: A multiplanar, lateral brow, temporal, and upper face lift. Plast. Reconstr. Surg. 97: 928, 1996.
From the Division of Plastic and Reconstructive Surgery, Brown University.
Received for publication August 30, 2004; revised October 22, 2004.
Presented in part at the 65th Annual Meeting of the American Society of Plastic and Reconstructive Surgeons, in Dallas, Texas, November 12, 1996.
Readers may also refer to the online version of the article at the Journal’s Web site (www.plasreconsurg.org) for additional materials.
Copyright ©2005 by the American Society of Plastic Surgeons
DOI: 10.1097/01.prs.0000185862.37301.32
www.plasreconsurg.org
